‘Overwhelmed’ health care workers share stories of professional pandemic perils
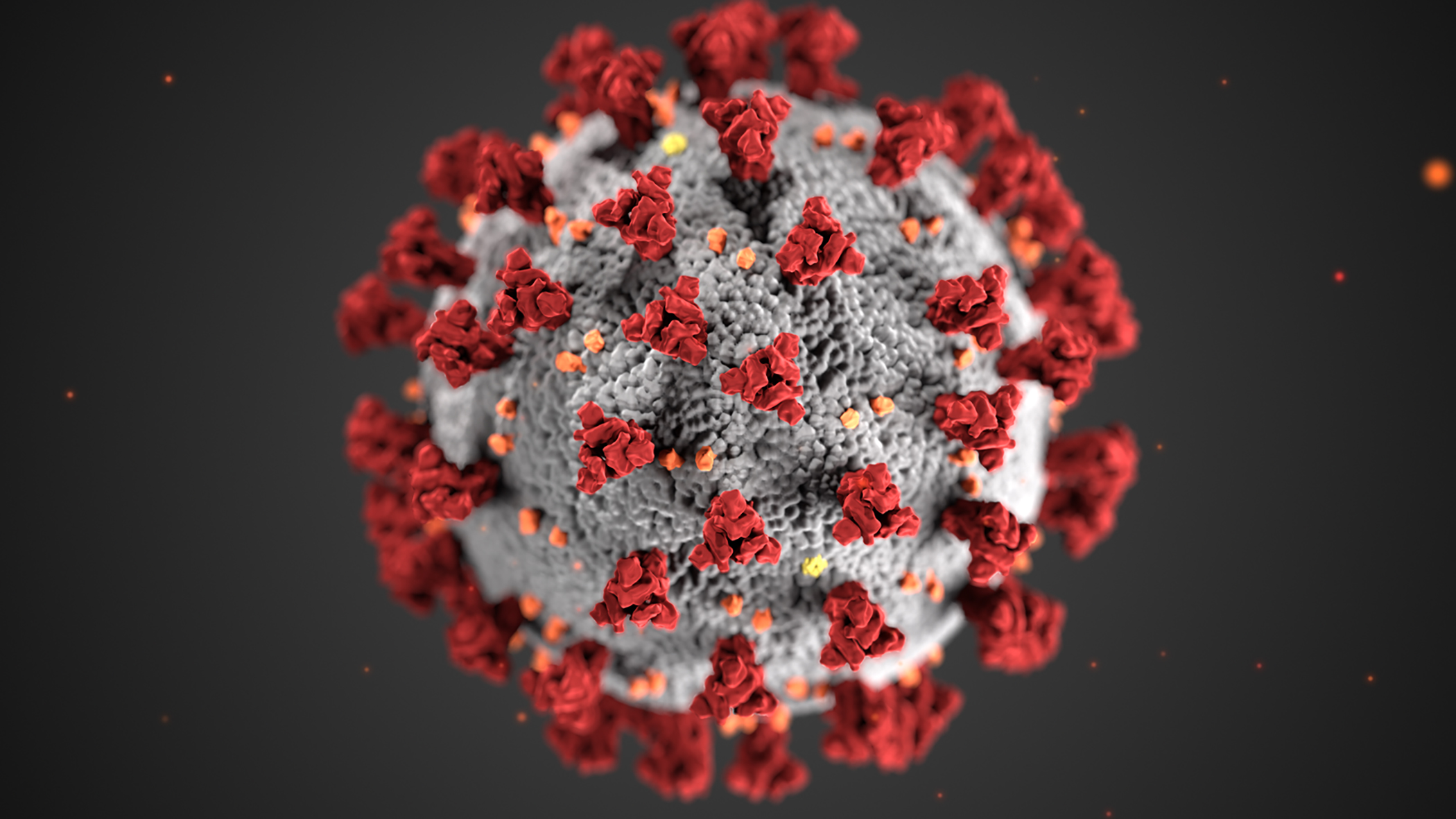
With the COVID-19 omicron variant rapidly spreading across the country, its effect on health care systems has been devastating.
But how bad is it in Minnesota for those working on the front lines?
“We’re just simply overwhelmed,” said Rachel Hanneman, a registered nurse. “We don’t often eat on our shifts because we can’t jeopardize our patient’s survival and our patient’s outcome to step away from the floor to do that. We don’t often drink because no one wants to remove their mask and risk contamination.” Working 12- and 16-hour shifts is common.
Hanneman likens the current situation to an eighth-grade shop class.
“Everyone was given the same amount of balsa wood, which is the flimsiest, almost foam-type of wood, but we were instructed to make a bridge out of it and see whose bridge could hold the most weight before it crashed,” she said. “The bridges that were the best reinforced ones, that had the best support, never broke at all. They held a substantial load. Most of those bridges broke. Right now, I feel like we are playing a very dangerous game where we are all doing that assignment. … We are using essential workers and essential professions instead of bridges and we’re finding how much pressure they can take before we’re willing to break.”
Hers was one observation the House Health Finance and Policy Committee heard Thursday from state health officials and other medical professionals on the extent of what is happening. No action was taken.
“The attempt we’re making is to give the public more of a window into what is really going on because we’re in a situation where we need everyone’s help. We need to really come together and fight this pandemic together,” said Rep. Tina Liebling (DFL-Rochester), the committee chair.
“It is not enough to simply say ‘thank you,’” said Rep. Liz Boldon (DFL-Rochester), a nurse for about 20 years.
Health Commissioner Jan Malcolm said the numbers, at the moment, remain troubling.
“It’s sort of the perfect storm,” she said. “An already taxed system, a tsunami of cases, a lower proportion of which would still net more numbers needing hospitalization at a time when staffing is lower than it has been and the system is incredibly, incredibly stressed from this long and arduous marathon that they continue to run on our behalf.”
Thursday's COVID-19 update from the department shows 11,510 newly reported cases and 52 newly reported deaths in a 24-hour period ending at 4 a.m. Wednesday. Minnesota's test positivity rate on a seven-day rolling average is a record-high 20.7%. Also released Thursday, the department’s weekly COVID-19 report shows numbers moving the wrong way.
“The good news is the illness appears to be milder in most people, but just as a factor of sheer numbers we will continue to see high hospitalizations,” Malcolm said, urging people get vaccinated. “Booster doses really, really do help in providing protection against hospitalization.”
Like everyone else, health care professionals are contracting COVID-19, which, coupled with things like burn out and vaccine mandates, leads to extraordinary staffing shortages in health care facilities.
And dwindling hope among employees.
“We are far enough into this pandemic to face the true reality there isn’t any more help coming,” said Kelley Anaas, an ICU nurse. “But the front line, the only line, still needs support and incentives to keep going. We need those in the position of power to see our humanity, recognize our limits and fill our cups so we can keep pouring from them.”
Gov. Tim Walz announced Wednesday that he intends to shift $40 million to help emergency hospital staffing. The decision will aim to cover provider costs associated with emergency staffing support and allow 350 temporary workers — primarily nurses — to work 60 hours a week for 60 days in hospitals around Minnesota. The dollars would come from a federal allocation to the state for pandemic aid.
Anaas has concerns, for example a fill-in not knowing where supplies are kept or which specialist to page in the middle of the night.
“Right now, travel nurses are a Band-Aid on a bullet wound,” she said. “We need to stop the bleed.”
Additionally, the governor noted the Department of Health is “taking emergency action to provide regulatory relief to hospitals and long-term care facilities, allowing them to expand capacity to more easily treat additional patients.” This includes waiving some fees and restrictions to add beds, permitting expanded capacity and allowing nursing homes to move or transfer patients without normal transfer and waiting periods.
Earlier in the day, the Senate Human Services Reform Finance and Policy Committee held an informational hearing on long-term care staffing shortages. (Watch the meeting)
“We are no longer in crisis; we are on the brink of collapse,” said Kari Thurlow, president and CEO of LeadingAge Minnesota, who said without emergency aid many nursing homes would have closed, especially those without a corporate infrastructure for support. “… The acute staffing crisis does lead to historically low occupancy and makes it very difficult to continue to operate.”
Related Articles
Search Session Daily
Advanced Search OptionsPriority Dailies
Speaker Emerita Melissa Hortman, husband killed in attack
By HPIS Staff House Speaker Emerita Melissa Hortman (DFL-Brooklyn Park) and her husband, Mark, were fatally shot in their home early Saturday morning.
Gov. Tim Walz announced the news dur...
House Speaker Emerita Melissa Hortman (DFL-Brooklyn Park) and her husband, Mark, were fatally shot in their home early Saturday morning.
Gov. Tim Walz announced the news dur...
Lawmakers deliver budget bills to governor's desk in one-day special session
By Mike Cook About that talk of needing all 21 hours left in a legislative day to complete a special session?
House members were more than up to the challenge Monday. Beginning at 10 a.m...
About that talk of needing all 21 hours left in a legislative day to complete a special session?
House members were more than up to the challenge Monday. Beginning at 10 a.m...